Is Lp(a) your missing risk predictor?
Lp(a) is nothing new, but its importance is breaking news. With a simple blood test performed only once in a patient’s lifetime, you can gain insight into their medical history, promote heart health, and anticipate potential risks.1

Menu
Hear the expert share his view on Lp(a)

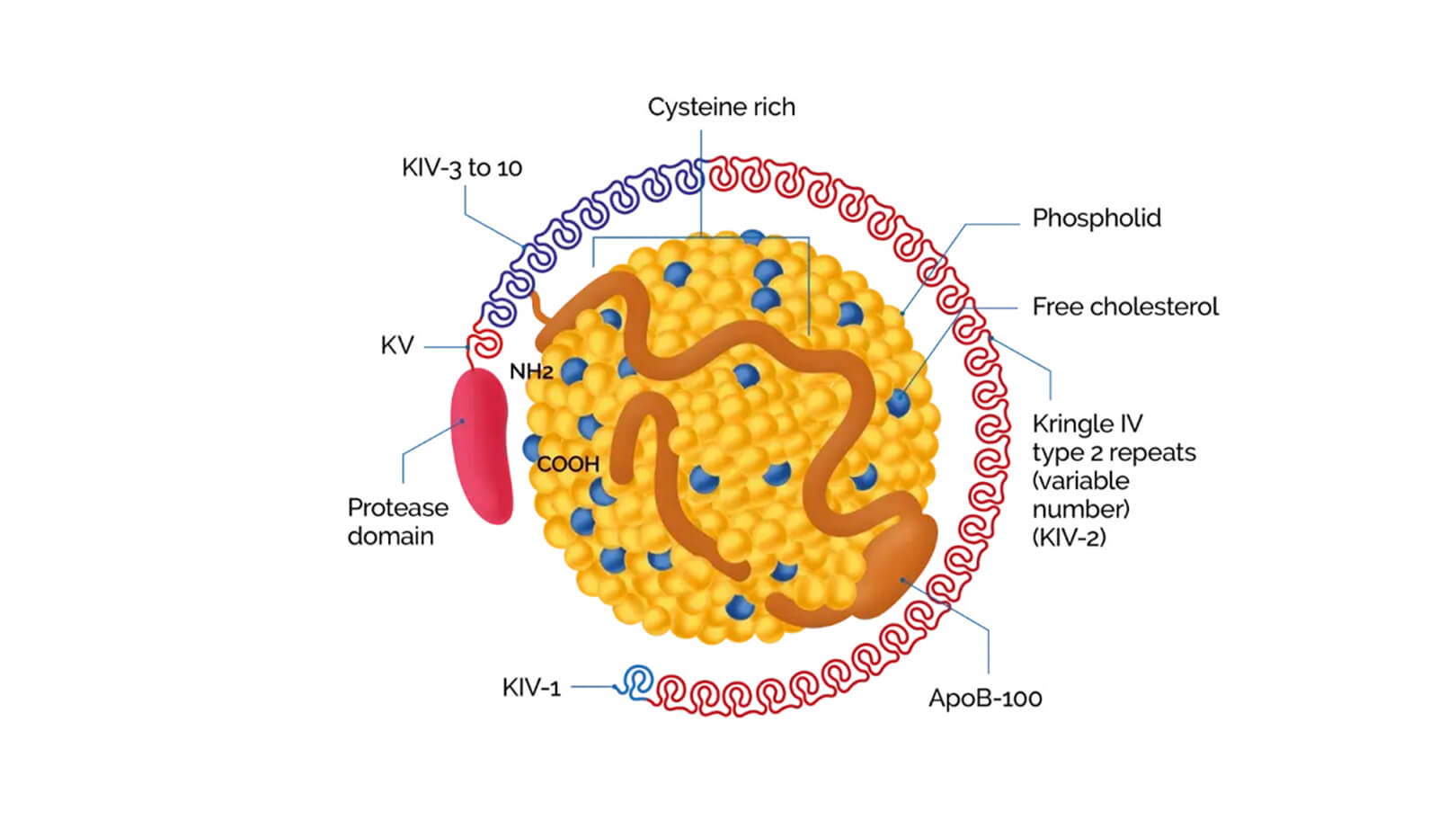
What is Lp(a)?
Listen to Børge Nordestgaard, Clinical Professor at University of Copenhagen, discuss the importance of identifying elevated Lp(a), a genetically determined condition that independently increases CVD risk.2
Stay in the know, sign up for our newsletter sign up here.
Take the Quiz on Lp(a)
Find more information about Lp(a) here
Common questions about Lp(a)13
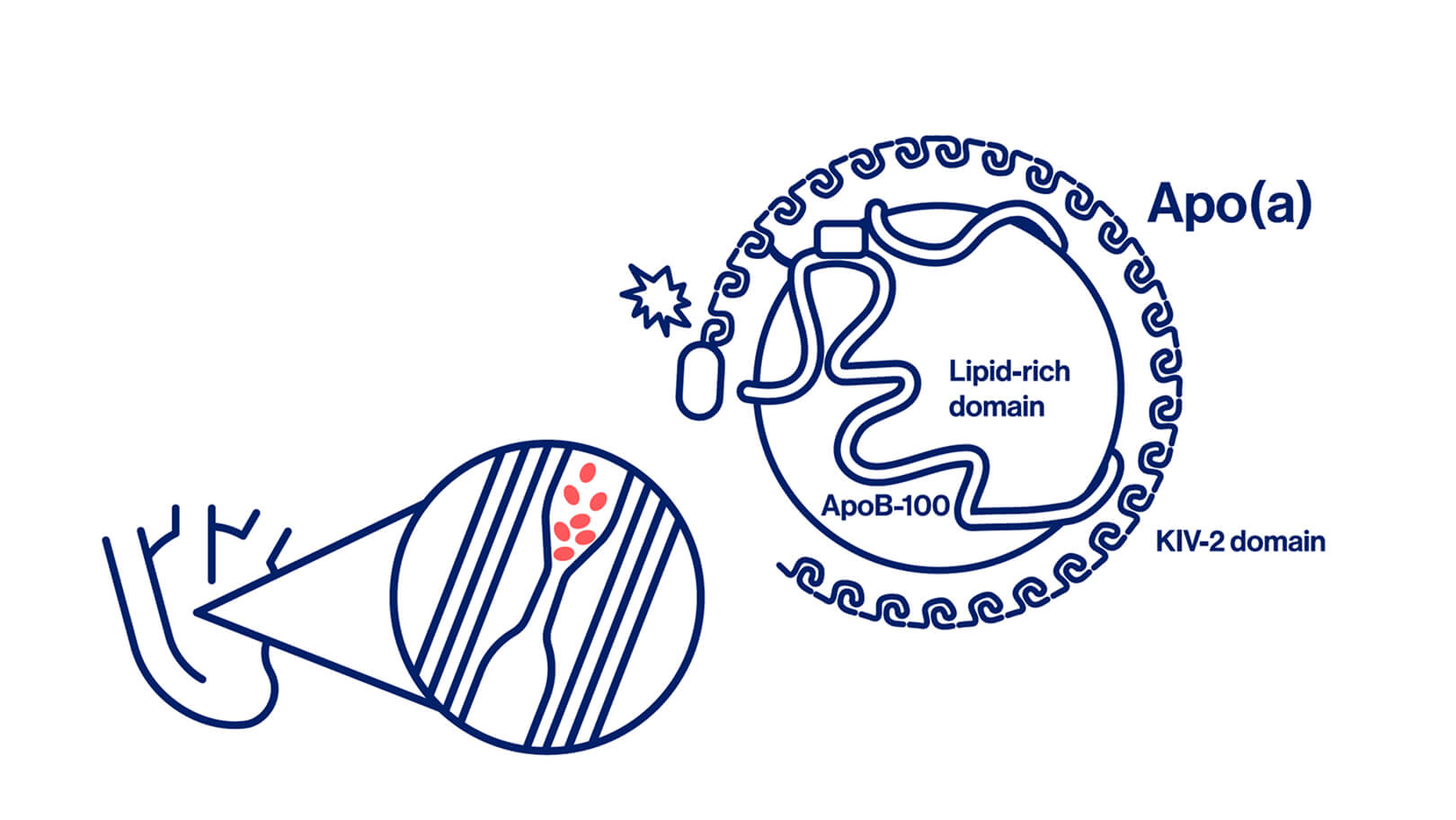
Lp(a) concentration is under strict genetic control, more so than any other lipoprotein, leaving limited room for other determinants. About 90% of plasma Lp(a) concentration is genetically determined and therefore hereditary. In contrast to genetic determinants, modifiable lifestyle factors (diet and physical activity) do not have a major influence on plasma Lp(a) concentration.13
Epidemiological, Mendelian randomisation, and genetic studies have demonstrated a causal relationship between elavated Lp(a) concentrations and ASCVD.13
Early and intensified risk factor management is, according to European guidelines, recommended for individuals with elevated Lp(a), taking into account their absolute global cardiovascular risk and the Lp(a) level.13,14
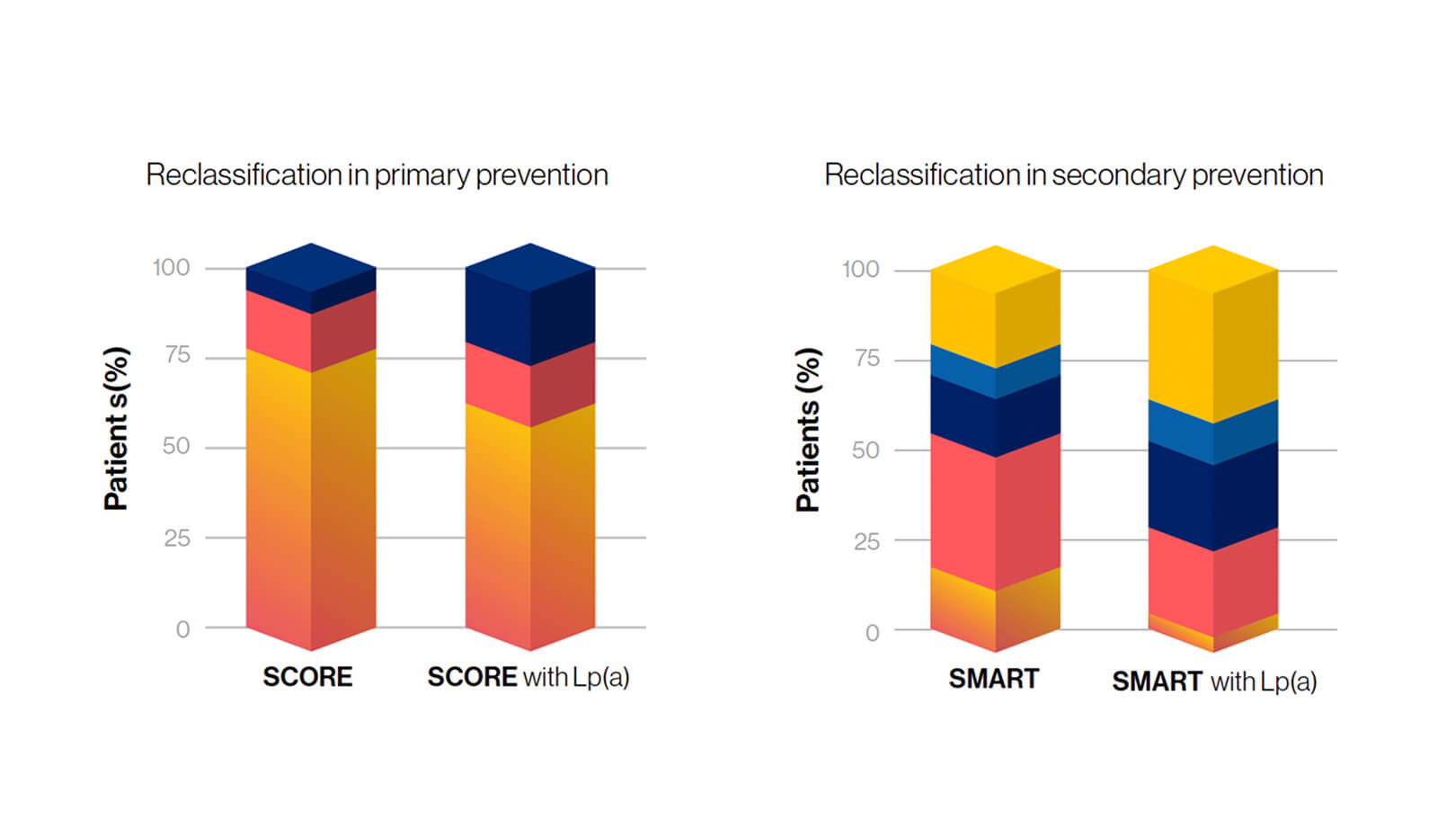
Yes; neglecting Lp(a) might result in a marked underestimation of risk for cardiovascular disease.13
No, there are differences. The strongest associations are seen for MI and aortic valve stenosis, with weaker associations for heart failure, ischemic stroke, and peripheral arterial disease.13
Yes, Lp(a) is a genetic driver of increased CVD risk that is independent of the risk conferred by LDL-C.13
Yes, in most people a single life-time measurement is sufficient since Lp(a) remain relatively constant over a lifetime.13
Management of other modifiable risk factors by lifestyle intervention and medical treatment according to guidelines is essential.13
Get the latest updates sign up for our newsletter
|
|
|
|
Referenser
- Kronenberg F, Mora S, Stroes ESG, et al. Lipoprotein(a) in atherosclerotic cardiovascular disease and aortic stenosis: a European Atherosclerosis Society consensus statement. Eur Heart J. 2022;43(39):3925-3946.
- Nordestgaard BG, Langsted A. Lipoprotein(a) and cardiovascular disease. Lancet. 2024;404(10459):1255-1264.
- Mehta A, Jain V, Saeed A, et al. Lipoprotein(a) and ethnicities. Atherosclerosis. 2022;349:42-52.
- Reyes-Soffer G, Yeang C, Michos ED, Boatwright W, Ballantyne CM. High lipoprotein(a): Actionable strategies for risk assessment and mitigation. Am J Prev Cardiol. 2024;18:100651.
- van der Valk FM, Bekkering S, Kroon J, et al. Oxidized Phospholipids on Lipoprotein(a) Elicit Arterial Wall Inflammation and an Inflammatory Monocyte Response in Humans. Circulation. 2016;134(8):611-624.
- Schnitzler JG, Hoogeveen RM, Ali L, et al. Atherogenic Lipoprotein(a) Increases Vascular Glycolysis, Thereby Facilitating Inflammation and Leukocyte Extravasation. Circ Res. 2020;126(10):1346-1359.
- Nurmohamed NS, Kaiser Y, Schuitema PCE, et al. Finding very high lipoprotein(a): the need for routine assessment. Eur J Prev Cardiol. 2022;29(5):769-776.
- Kaiser Y, Daghem M, Tzolos E, et al. Association of Lipoprotein(a) With Atherosclerotic Plaque Progression. J Am Coll Cardiol. 2022;79(3):223-233.
- Leistner DM, Laguna-Fernandez A, Haghikia A, et al. Impact of elevated lipoprotein(a) on coronary artery disease phenotype and severity. Eur J Prev Cardiol. 2024;31(7):856-865.
- Kato A, Kinoshita D, Nagata T, et al. Lipoprotein (a) levels and vulnerable characteristics in nonculprit plaque in patients with acute coronary syndrome. Int J Cardiol Heart Vasc. 2022;43:101120.
- Verweij SL, de Ronde MWJ, Verbeek R, et al. Elevated lipoprotein(a) levels are associated with coronary artery calcium scores in asymptomatic individuals with a family history of premature atherosclerotic cardiovascular disease. J Clin Lipidol. 2018;12(3):597-603.e1.
- Garg PK, Guan W, Karger AB, Steffen BT, Budoff M, Tsai MY. Lipoprotein (a) and risk for calcification of the coronary arteries, mitral valve, and thoracic aorta: The Multi-Ethnic Study of Atherosclerosis. J Cardiovasc Comput Tomogr. 2021;15(2):154-160.
- Kronenberg F, Mora S, Stroes ESG, et al. Frequent questions and responses on the 2022 lipoprotein(a) consensus statement of the European Atherosclerosis Society. Atherosclerosis. 2023;374:107-120.
- Mach F et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk, Atherosclerosis 290 (2019) 140–205.